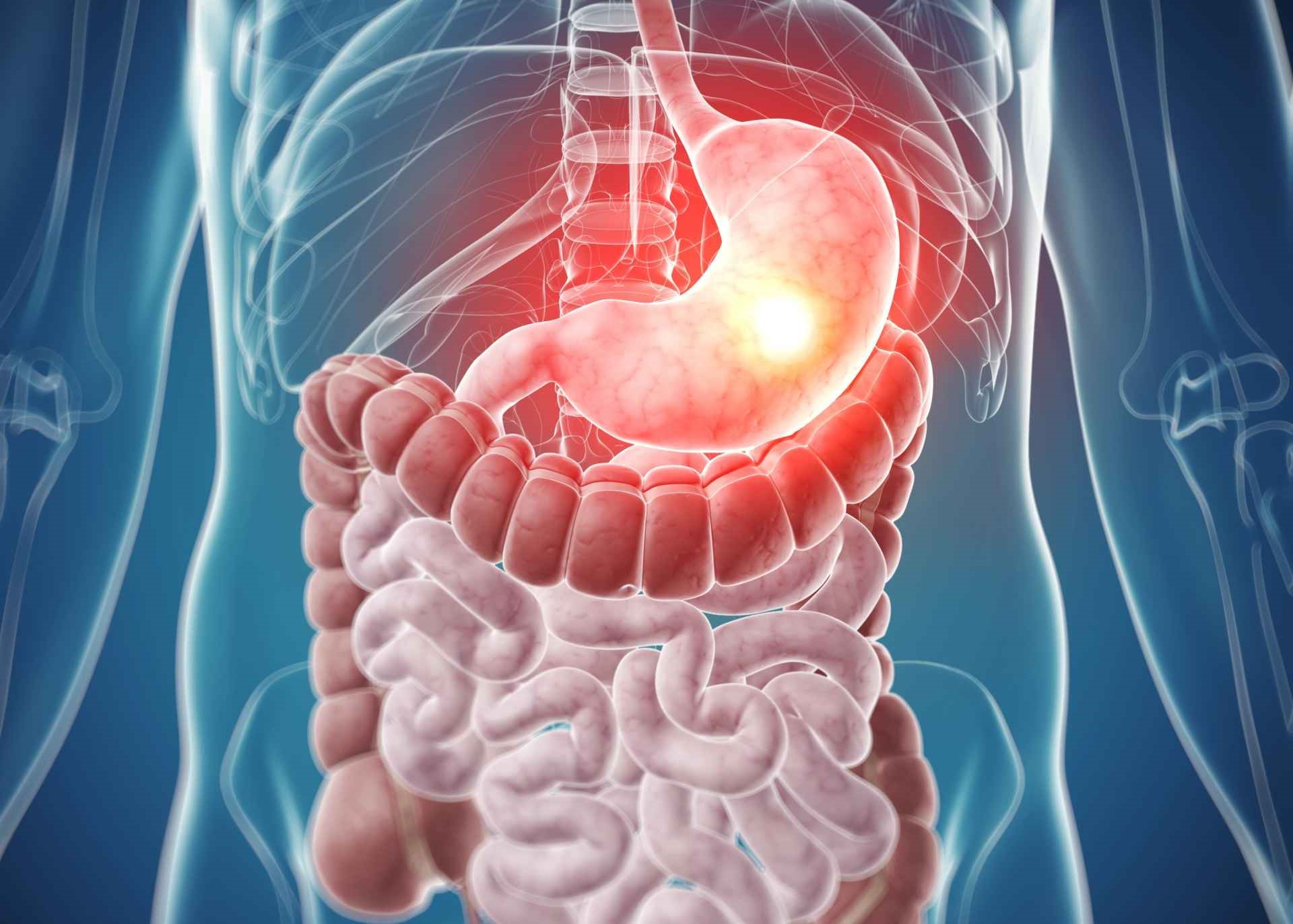
Whenever open sores, or ulcers, grow in the stomach or the first segment of the small intestine, peptic ulcer symptoms appear. Peptic ulcer condition is caused by a bacterial infection that chips away at the primary layer of the digestive system. Individuals who receive pain relievers frequently are more likely to acquire ulcers. Based on the area, this condition can be gastric. It’s a stomach ulcer if the ulcer damages the stomach. A duodenal ulcer infects the first segment of the small intestine.
Symptoms of Peptic Ulcers
The most typical sign of a peptic ulcer is discomfort. It is usually felt in the top portion of the belly, between the breastbone and the navel, but it can also be felt in the rear. Your discomfort may be dull, searing, or tormenting; it’s less likely that it’s acute or stabbing. The discomfort is usually worse at night or first thing in the morning, but this might vary. Pain might last anywhere from a few minutes to several hours.
On an empty belly, most individuals with peptic ulcers experience severe agony. You may feel better just after dining, only to have the discomfort return or intensify an hour later. Individuals with ulcers, on the other hand, do not overeat during this brief respite since recurrent nausea and suffering can suppress appetite and the urge to eat. Certain people believe that particular foods (such as fatty foods) aggravate symptoms, while others believe that other food products either ease or have no effect. Although pain is by far the most prevalent sign, more than half of those who have peptic ulcers have no indications at all.
- Vomits (with or without blood)
- Feces with blood in it; dark and tarry stool
- Tiredness or weakness, which might be caused by malnutrition or anemia caused by modest amounts of ulcer bleeding.
- Weight loss
- A steady bleed from an ulcer might occur without creating major symptoms. It’s possible that it won’t create any signs at all. Anemia could only be detected through blood tests. An individual with anemia may also experience weariness, pale complexion, and shortness of breath in some circumstances.
- If the bleeding is severe, the person may lose a lot of blood in a short period, resulting in black, brown, or dark red feces. Blood, either fresh and brilliant red or dark and like coffee beans, might be vomited. This is a life-threatening emergency that necessitates hospitalization and treatment.
- Due to a lack of food consumption, the patient may become vitamin and mineral poor. Malnutrition can cause immune inadequacies, bone weakening, and skin fragility, all of which may not be obvious at first. Malnutrition, on the other hand, is not a prevalent consequence of peptic ulcers in today’s environment.
- A perforated ulcer is a medical issue in and of itself. When the stomach contents flow into the abdominal wall, an infection can result. The signs are more acute, with a quick onset of strong, excruciating abdominal discomfort. Any mobility exacerbates the problem. Septic shock can result from a perforated ulcer, which causes a rise in heart rate, a reduction in blood pressure, and the incapacity to pee.
In essence, peptic ulcers could be divided into two types. One type is known as stomach ulcers, while the others are known as duodenal ulcers. Stomach ulcers form on the inside of the belly in gastric ulcers. Duodenal ulcers, on the other hand, originate on the inside of the initial section of the small intestine, the duodenum.
Cause of Peptic Ulcers
Ulcers are commonly believed to be due to stress or the consumption of certain foods. Experts, on the other hand, have found no evidence to support such ideas. The bacteria Helicobacter pylori (H. pylori) and long-term utilization of nonsteroidal anti-inflammatory medicines are the most likely reasons for peptic ulcers (NSAIDs).
Helicobacter pylori
It is a common bacterial infection of the gastrointestinal tract. About half of the world’s population is infected with H. pylori, which often goes unnoticed. It appears to be transmissible from individual to individual, especially throughout childhood, according to studies. The existence of H. pylori, on the other hand, has no negative impact on the majority of people. Only about 10% to 15% of people who are infected with H. pylori create ulcers.
Anti-inflammatory medications
Another common cause of peptic ulcer illness is the use of nonsteroidal anti-inflammatory drugs (NSAIDs). The mucus covering the digestive tract may be worn away by NSAIDs. Peptic ulcers could be caused by aspirin, naproxen, ibuprofen, and prescription NSAIDs. Not everybody who uses nonsteroidal anti-inflammatory drugs (NSAIDs) develops ulcers. The most dangerous combination is NSAID use along with H. pylori infection. People with H. pylori who take NSAIDs regularly are more prone to have their mucus layer destroyed, and the damage can be serious.